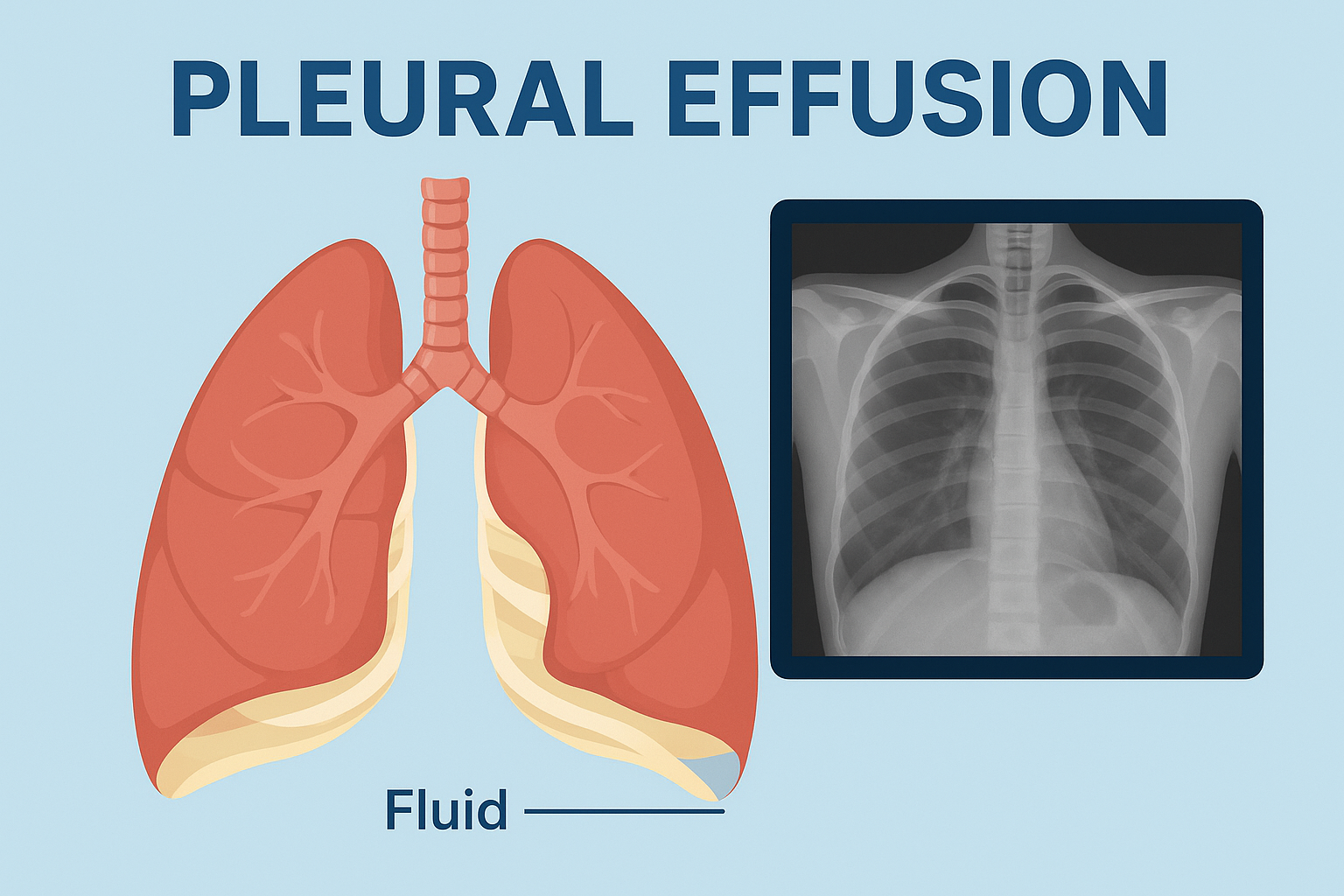
Pleural effusion, commonly known as “fluid on the lungs,” is a medical condition in which an abnormal amount of fluid builds up between the layers of the pleura—the thin membranes that line the lungs and chest cavity. This condition can affect breathing, cause discomfort, and may indicate an underlying disease.
In this blog, we will discuss the causes, symptoms, diagnosis, complications, and treatment of pleural effusion, along with preventive aspects to raise awareness.
What is Pleural Effusion?
The pleural space normally contains a small amount of lubricating fluid that allows smooth lung expansion during breathing. In pleural effusion, excessive fluid accumulates in this space, which can restrict lung movement and impair normal breathing.
Types of Pleural Effusion
Pleural effusion is broadly classified into two main types:
- Transudative Effusion
- Caused by fluid leakage due to increased pressure or low protein levels.
- Commonly associated with heart failure, cirrhosis, and kidney disease.
- Exudative Effusion
- Caused by inflammation, infection, or malignancy.
- Seen in pneumonia, tuberculosis, pulmonary embolism, and cancers.
Causes of Pleural Effusion
Pleural effusion may occur due to various medical conditions, including:
- Congestive heart failure (most common cause)
- Pneumonia and lung infections
- Tuberculosis (TB)
- Cancer (lung cancer, breast cancer, lymphoma, etc.)
- Kidney or liver disease
- Pulmonary embolism (blood clot in the lungs)
- Autoimmune diseases such as lupus or rheumatoid arthritis
Symptoms of Pleural Effusion
Mild pleural effusion may not cause symptoms, but larger fluid accumulation can lead to:
- Shortness of breath (dyspnea)
- Chest pain or heaviness (worse with deep breaths)
- Dry cough
- Difficulty breathing while lying down
- Fatigue
Diagnosis of Pleural Effusion
Doctors use multiple methods to confirm pleural effusion:
- Chest X-ray: Shows fluid collection.
- Ultrasound: Detects even small amounts of fluid.
- CT scan: Provides detailed images of lungs and pleura.
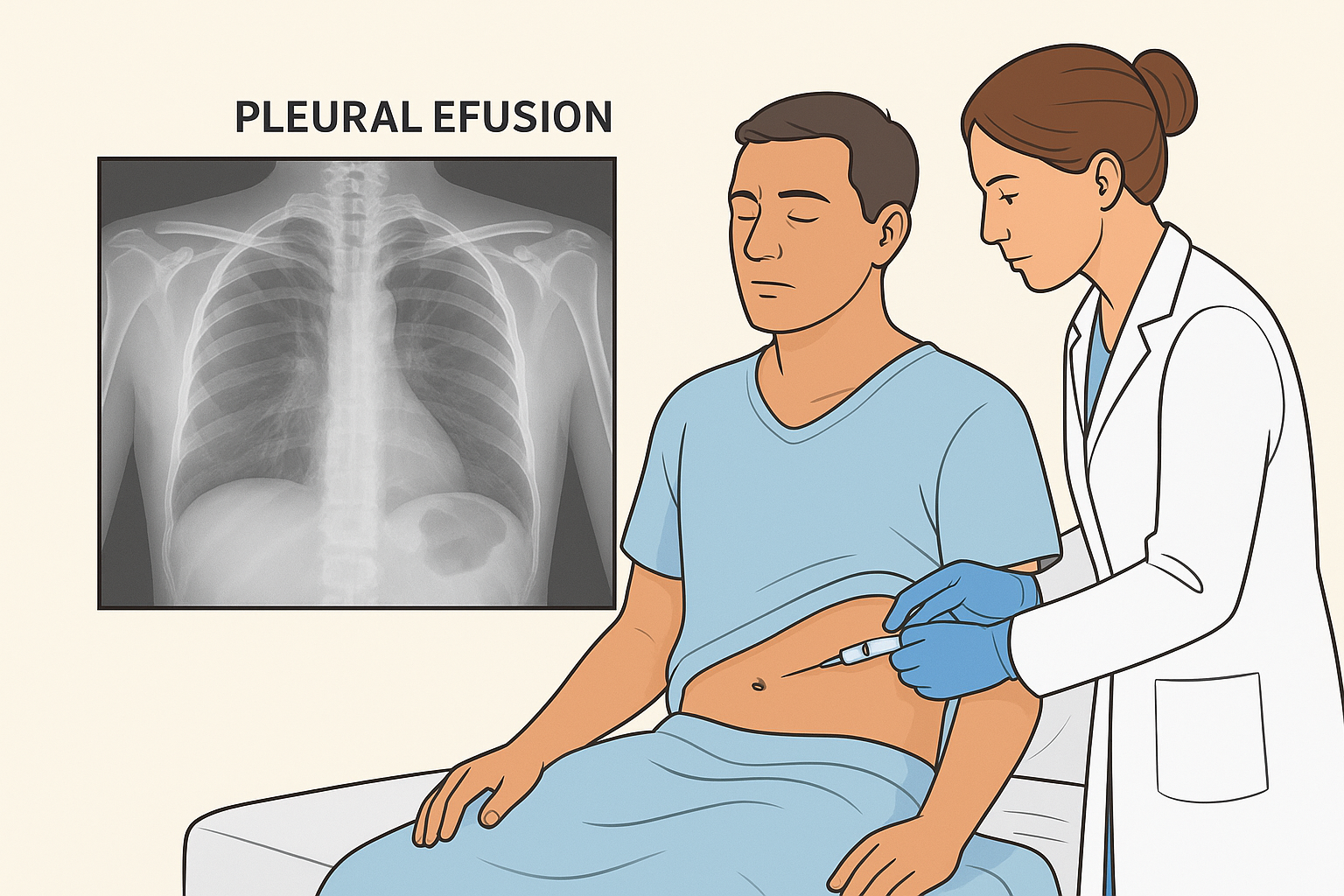
- Thoracentesis: A procedure to remove fluid for laboratory analysis.
Lab tests help differentiate between transudative and exudative effusion, guiding further treatment.
Complications of Pleural Effusion
If left untreated, pleural effusion may lead to:
- Collapsed lung (atelectasis)
- Empyema (infected pus-filled effusion)
- Sepsis (life-threatening infection spread)
- Respiratory failure in severe cases
Treatment of Pleural Effusion
Treatment depends on the cause, size, and severity of the effusion:
- Thoracentesis – A needle procedure to drain excess fluid.
- Chest Tube Insertion – For large or recurrent effusions.
- Medications:
- Diuretics for heart failure-related effusion.
- Antibiotics for infections.
- Anti-tuberculosis drugs for TB-related effusion.
- Pleurodesis – A procedure that seals the pleural space to prevent recurrence (often in cancer cases).
- Surgery – Sometimes needed for complex or persistent effusions.
Prevention and Lifestyle Management
While pleural effusion itself may not always be preventable, managing underlying conditions can reduce the risk. Key steps include:
- Regular treatment for heart, kidney, and liver diseases.
- Timely management of lung infections like pneumonia and TB.
- Regular medical check-ups if you have cancer or chronic illness.
- Avoiding smoking to reduce risk of lung diseases.
Key Takeaway
Pleural effusion is not a disease in itself but a sign of an underlying health problem. Identifying the cause early is crucial for effective treatment. With timely medical care, most patients can recover and prevent recurrence.
If you or someone you know is experiencing persistent shortness of breath, chest discomfort, or unexplained cough, seek medical advice immediately for early diagnosis and management.