Pleural effusion is a medical condition in which excess fluid accumulates between the layers of the pleura, the thin membranes that surround the lungs. Normally, only a small amount of lubricating fluid is present to allow smooth breathing movements, but when the fluid builds up excessively, it can cause breathing difficulties and discomfort. Pleural effusion is often a sign of an underlying disease and requires proper diagnosis and treatment.
What is Pleural Effusion?
The pleura is a two-layered membrane: one layer covers the lungs, while the other lines the chest cavity. A small amount of fluid is normally present between these layers. When this balance is disturbed, pleural effusion occurs, leading to restricted lung expansion and reduced oxygen intake.
Causes of Pleural Effusion
Pleural effusion can result from a variety of conditions. The two main types are:
- Transudative Effusion (low-protein fluid):
Caused by conditions that increase pressure or decrease protein levels in blood.- Heart failure
- Cirrhosis of the liver
- Kidney disease (nephrotic syndrome)
- Exudative Effusion (high-protein fluid):
Caused by inflammation, infection, or malignancy.- Pneumonia (parapneumonic effusion)
- Tuberculosis
- Lung cancer, breast cancer, or metastatic cancers
- Pulmonary embolism
- Autoimmune diseases (like lupus, rheumatoid arthritis)
Symptoms of Pleural Effusion
Some patients may have no symptoms if the fluid buildup is small. However, common signs include:
- Shortness of breath (dyspnea), especially on exertion
- Chest pain or heaviness (often worsens with deep breathing)
- Persistent dry cough
- Fever and night sweats (in infectious causes)
- Orthopnea (difficulty breathing while lying flat)
- Decreased breath sounds on the affected side
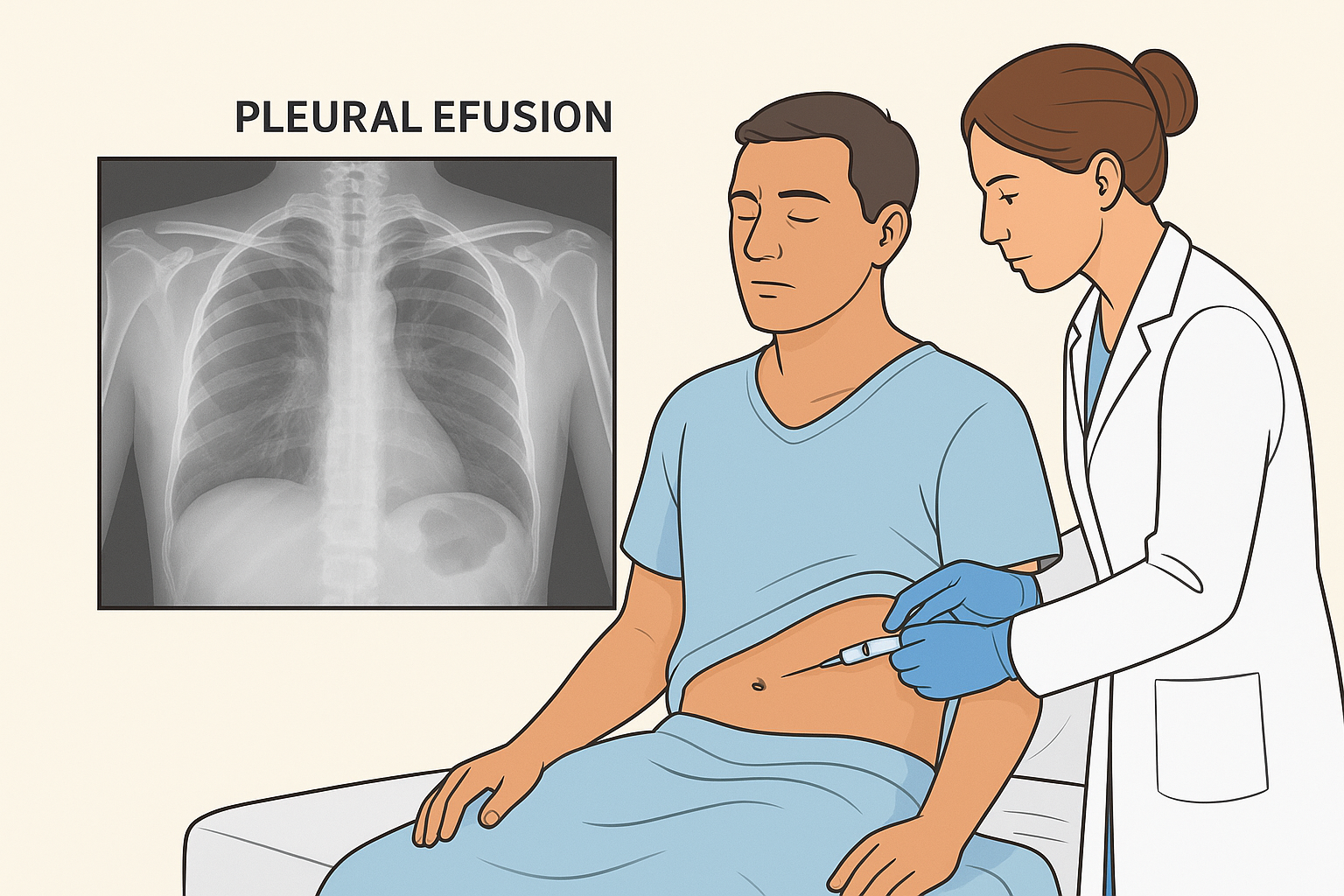
Diagnosis of Pleural Effusion
Doctors use several methods to diagnose pleural effusion and its cause:
- Physical Examination: Reduced chest movement, dullness to percussion, and decreased breath sounds.
- Chest X-ray: Shows fluid collection in the lungs.
- Ultrasound or CT Scan: Detects even small amounts of fluid and guides procedures.
- Thoracentesis (Pleural Tap): Fluid is removed with a needle and tested for infection, cancer, or protein levels.
- Blood Tests: To check for infections, autoimmune diseases, or organ dysfunction.
Treatment of Pleural Effusion
Treatment depends on the cause, severity, and recurrence of fluid buildup:
1. Therapeutic Thoracentesis
- Removes fluid to relieve symptoms and improve breathing.
2. Medications
- Diuretics: For effusions due to heart failure.
- Antibiotics: For pneumonia or tuberculosis-related effusion.
- Chemotherapy or targeted therapy: For malignant pleural effusion.
3. Chest Tube Drainage (Tube Thoracostomy)
- Used for large or recurrent effusions, particularly in infections or cancer.
4. Pleurodesis
- A medical procedure where chemicals (e.g., talc) are introduced into the pleural space to prevent fluid re-accumulation, commonly used in cancer patients.
5. Surgery (Decortication or Pleurectomy)
- In severe or resistant cases, surgery may be required to remove pleural tissue or peel off thickened pleura.
Complications of Pleural Effusion
If untreated, pleural effusion can lead to:
- Lung collapse (atelectasis)
- Empyema (collection of pus in pleural cavity)
- Sepsis (in case of infections spreading)
- Respiratory failure in severe cases
Prevention of Pleural Effusion
While not all cases can be prevented, reducing risk factors can lower the chances:
- Early treatment of chest infections (pneumonia, tuberculosis).
- Proper management of chronic diseases like heart failure and kidney disease.
- Regular cancer screening and follow-up in high-risk patients.
- Healthy lifestyle practices to support lung and heart function.
Final Thoughts
Pleural effusion is a serious condition that requires timely medical evaluation and treatment. It is often a sign of an underlying illness, such as infection, heart failure, or cancer. Early diagnosis, fluid analysis, and appropriate management are vital to prevent complications and restore breathing comfort.
Raising awareness about pleural effusion helps patients seek timely care and improves overall health outcomes.