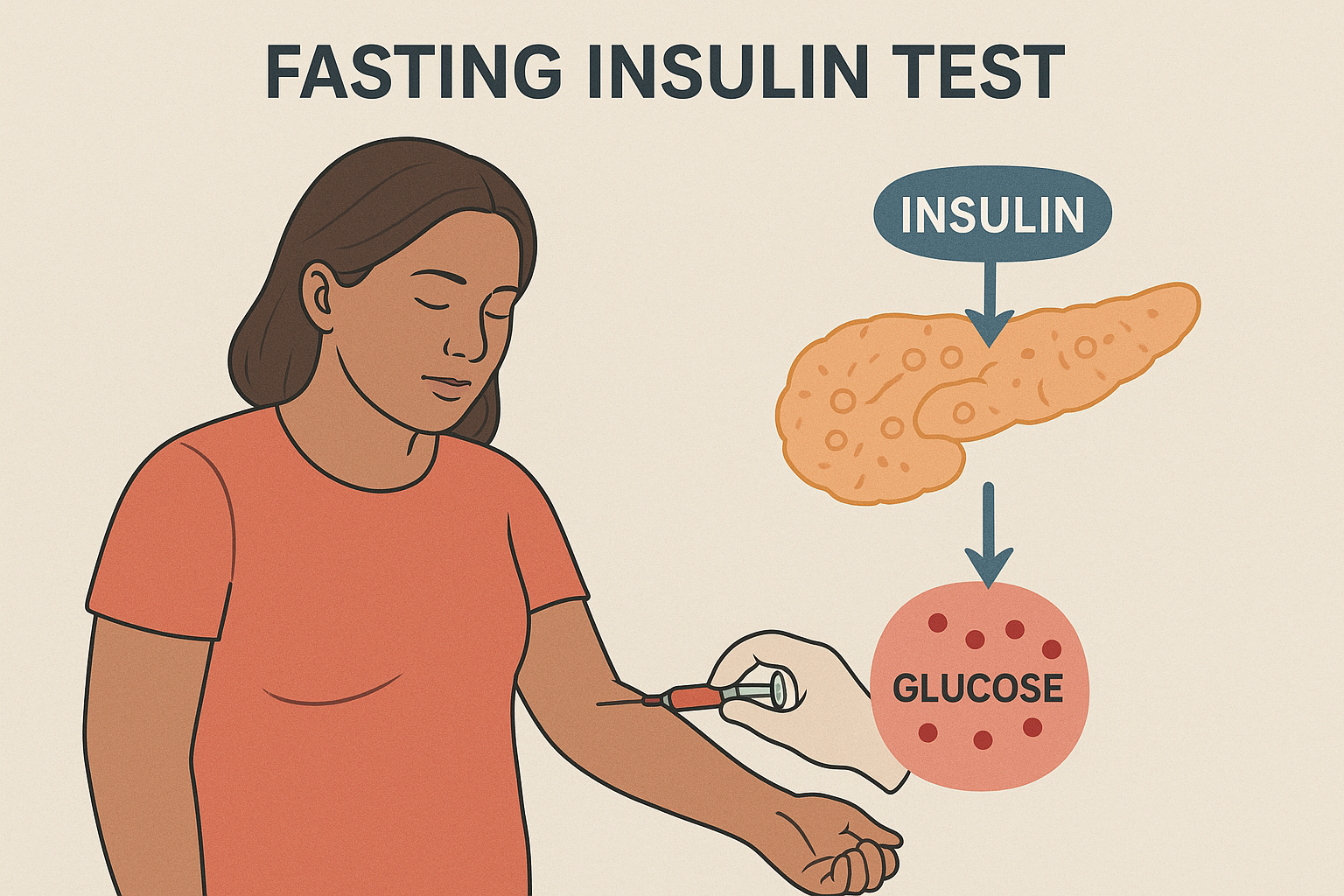
The fasting insulin test is a crucial blood test used to measure the amount of insulin in your body after an overnight fast. It helps doctors evaluate how well your body regulates blood sugar levels and whether you may have conditions like insulin resistance, prediabetes, or type 2 diabetes.
Insulin, produced by the pancreas, plays a key role in controlling blood glucose. Abnormal insulin levels can be early warning signs of metabolic disorders even before blood sugar levels rise.
What Is Fasting Insulin?
Fasting insulin refers to the insulin concentration in the blood after not eating for at least 8–12 hours.
It provides valuable insight into how efficiently your body maintains normal glucose levels in the fasting state.
If the body becomes insulin resistant, the pancreas compensates by producing more insulin. This can lead to elevated fasting insulin levels, even when glucose appears normal — a condition that often precedes diabetes.
Why Is the Fasting Insulin Test Important?
The fasting insulin test helps in:
- Detecting insulin resistance early (before blood sugar rises).
- Monitoring metabolic health in individuals at risk for diabetes.
- Evaluating hypoglycemia (low blood sugar) causes.
- Assessing pancreatic function in metabolic or endocrine disorders.
- Guiding treatment for obesity, metabolic syndrome, or polycystic ovary syndrome (PCOS).
Who Should Get a Fasting Insulin Test?
Doctors may recommend a fasting insulin test if you have:
- Family history of diabetes or metabolic syndrome
- Unexplained weight gain or difficulty losing weight
- Fatigue or frequent hunger
- High triglycerides and low HDL (good cholesterol)
- High blood pressure
- Acanthosis nigricans (dark skin patches on the neck or armpits)
- PCOS in women
How Is the Fasting Insulin Test Performed?
The procedure is simple and usually done in the morning after an overnight fast.
- Preparation:
- Do not eat or drink (except water) for 8–12 hours before the test.
- Avoid intense exercise or alcohol before testing.
- During the Test:
- A small blood sample is drawn from a vein in your arm.
- After the Test:
- You can resume normal activities and meals.
- The sample is analyzed in a laboratory to measure insulin levels.
Normal Fasting Insulin Levels
Normal values can vary slightly between laboratories, but generally:
| Status | Fasting Insulin Level (µIU/mL) |
|---|---|
| Normal | 2 – 10 |
| Borderline | 11 – 15 |
| High (Insulin Resistance) | > 15 |
High fasting insulin indicates insulin resistance, even if fasting glucose levels are within normal range.
Interpreting the Results
- Normal Insulin Levels:
Indicate proper insulin sensitivity and glucose metabolism. - Elevated Insulin Levels:
Suggest the pancreas is overworking to maintain blood sugar, which may indicate:- Insulin resistance
- Prediabetes
- Metabolic syndrome
- Obesity-related insulin overproduction
- PCOS (in women)
- Low Insulin Levels:
May indicate:- Type 1 diabetes
- Late-stage type 2 diabetes (when pancreas is exhausted)
- Pancreatic disorders
Relation Between Fasting Insulin and HOMA-IR
HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) is a formula that combines fasting glucose and fasting insulin to estimate insulin resistance: HOMA-IR=(Fasting Insulin µIU/mL×Fasting Glucose mg/dL)405\text{HOMA-IR} = \frac{(\text{Fasting Insulin µIU/mL} \times \text{Fasting Glucose mg/dL})}{405}HOMA-IR=405(Fasting Insulin µIU/mL×Fasting Glucose mg/dL)
- HOMA-IR < 2.0 → Normal
- HOMA-IR 2.0–2.9 → Borderline insulin resistance
- HOMA-IR ≥ 3.0 → Insulin resistance present
This index is widely used in research and clinical practice to assess metabolic health.
How to Improve Fasting Insulin Levels
Maintaining healthy insulin levels involves lifestyle changes that improve insulin sensitivity:
1. Eat a Balanced, Low-Glycemic Diet
- Choose whole grains, lean proteins, and fiber-rich foods.
- Limit refined sugars, sweetened beverages, and processed foods.
2. Exercise Regularly
- Engage in aerobic exercises (walking, jogging, cycling) and resistance training.
- Physical activity helps muscles use glucose more effectively.
3. Maintain a Healthy Weight
- Even a 5–10% weight reduction can lower fasting insulin significantly.
4. Manage Stress
- Chronic stress elevates cortisol, which increases insulin levels.
- Practice relaxation techniques like yoga, deep breathing, or meditation.
5. Get Adequate Sleep
- Poor sleep contributes to insulin resistance and higher fasting insulin levels.
6. Medical Treatment
- Metformin may be prescribed for patients with insulin resistance or prediabetes.
- Always follow your doctor’s advice for personalized treatment.
Conclusion
A fasting insulin test is a valuable tool for assessing metabolic health and detecting insulin resistance early — before serious conditions like diabetes develop.
Regular monitoring, healthy eating, exercise, and stress management can help maintain normal insulin function and prevent long-term complications.
Understanding your fasting insulin levels empowers you to take control of your health, energy, and longevity.