Hypertension, commonly known as high blood pressure, is a major global health concern that significantly increases the risk of heart disease, stroke, kidney failure, and other cardiovascular complications. With ongoing research, the classification of hypertension has evolved to reflect the latest evidence on diagnosis, risk assessment, and management. The latest classification, based on the American College of Cardiology (ACC), American Heart Association (AHA), and World Health Organization (WHO) guidelines, helps in early detection and better control of blood pressure.
What Is Hypertension?
Hypertension is a chronic medical condition in which the force of blood against the artery walls is consistently too high.
Blood pressure (BP) is expressed in two readings:
- Systolic BP (SBP): The pressure when the heart contracts
- Diastolic BP (DBP): The pressure when the heart relaxes
A normal blood pressure ensures that the body’s organs receive an adequate supply of oxygen and nutrients. However, when BP remains elevated over time, it damages blood vessels and vital organs.
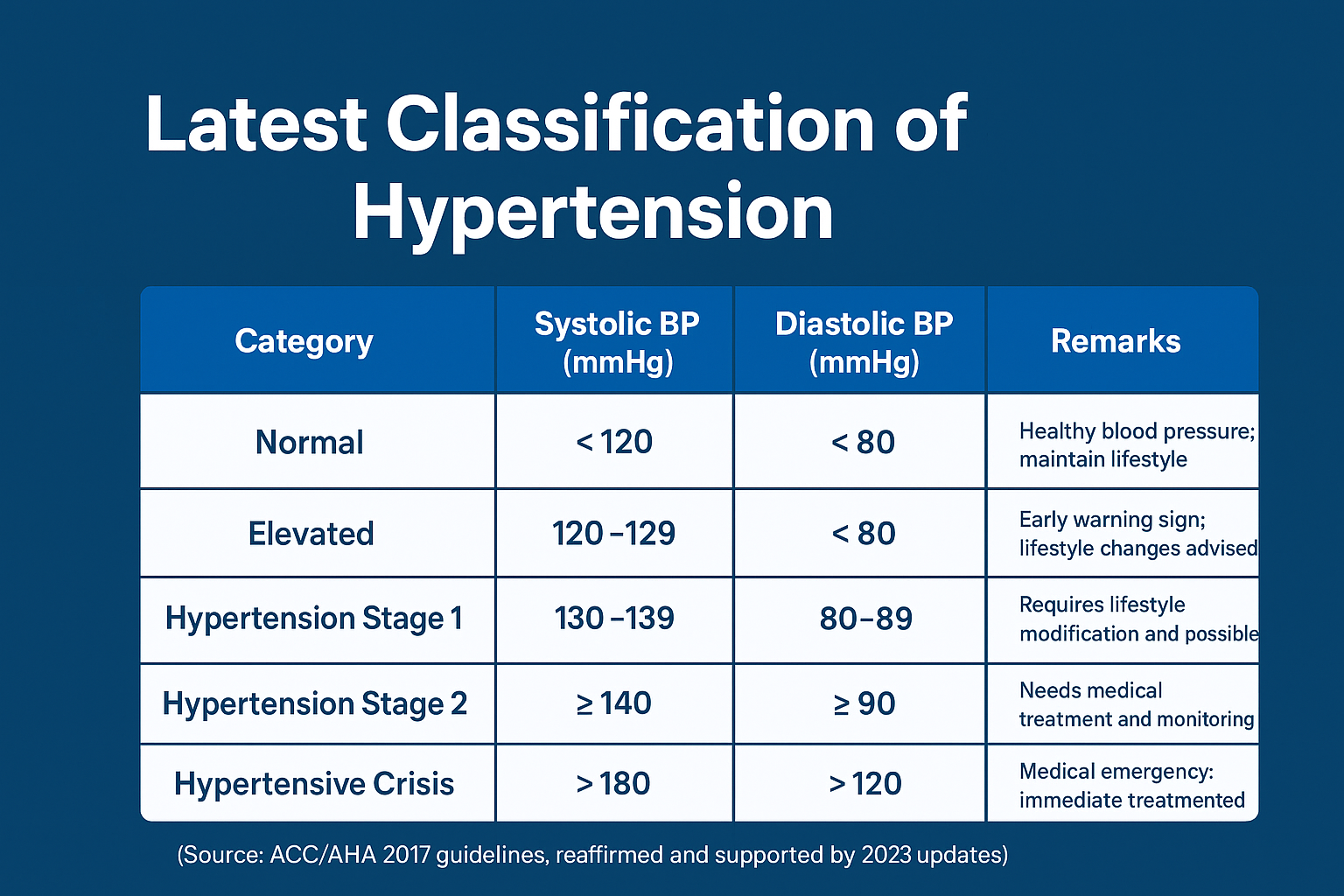
Latest Classification of Hypertension (According to 2023–2024 Guidelines)
The latest classification focuses on precise blood pressure ranges, early intervention, and individualized treatment.
| Category | Systolic BP (mmHg) | Diastolic BP (mmHg) | Remarks |
|---|---|---|---|
| Normal | < 120 | < 80 | Healthy blood pressure; maintain lifestyle |
| Elevated | 120–129 | < 80 | Early warning sign; lifestyle changes advised |
| Hypertension Stage 1 | 130–139 | 80–89 | Requires lifestyle modification and possible medication |
| Hypertension Stage 2 | ≥ 140 | ≥ 90 | Needs medical treatment and monitoring |
| Hypertensive Crisis | > 180 | > 120 | Medical emergency; immediate treatment required |
(Source: ACC/AHA 2017 guidelines, reaffirmed and supported by 2023 updates)
WHO and International Classifications
The World Health Organization (WHO) and International Society of Hypertension (ISH) have also refined their 2021–2024 classification, which closely aligns with the ACC/AHA system but emphasizes risk-based assessment.
- WHO recommends a global threshold of ≥140/90 mmHg for diagnosis.
- It highlights the importance of home and ambulatory BP monitoring for accuracy.
Subtypes of Hypertension
Hypertension can also be classified based on underlying causes and patterns:
1. Primary (Essential) Hypertension
- Accounts for 90–95% of all cases.
- No identifiable cause; associated with genetic, environmental, and lifestyle factors (salt intake, obesity, stress, lack of exercise).
- Develops gradually over years.
2. Secondary Hypertension
- Occurs due to identifiable underlying conditions such as:
- Chronic kidney disease
- Endocrine disorders (Cushing’s syndrome, hyperthyroidism, pheochromocytoma)
- Medications (steroids, oral contraceptives, NSAIDs)
- Sleep apnea
Treating the underlying cause often helps control BP effectively.
3. Isolated Systolic Hypertension
- Systolic BP ≥ 140 mmHg with normal diastolic BP (<90 mmHg)
- Common in older adults due to arterial stiffness
- Requires careful management to prevent cardiovascular complications
4. White Coat and Masked Hypertension
- White Coat Hypertension: High BP only in a clinical setting due to anxiety.
- Masked Hypertension: Normal BP in clinic but elevated at home.
Both conditions require home BP monitoring or ambulatory BP monitoring for accurate diagnosis.
Hypertension in Special Populations
- Pregnancy: May present as gestational hypertension or preeclampsia, requiring close monitoring.
- Elderly: More prone to isolated systolic hypertension.
- Diabetics and CKD patients: Target BP is lower (<130/80 mmHg) for better outcomes.
Management Overview
The cornerstone of hypertension management includes:
- Lifestyle modifications: Reduced salt intake, regular exercise, weight control, and stress reduction.
- Medications: ACE inhibitors, ARBs, calcium channel blockers, diuretics, and beta-blockers as per patient profile.
- Regular monitoring: Routine BP checks help prevent complications.
Conclusion
The latest classification of hypertension emphasizes early identification and proactive management. Recognizing elevated blood pressure before it reaches dangerous levels can significantly reduce the risk of heart attack, stroke, and kidney disease.
Following the updated guidelines ensures better control, improved health outcomes, and personalized treatment for every patient.