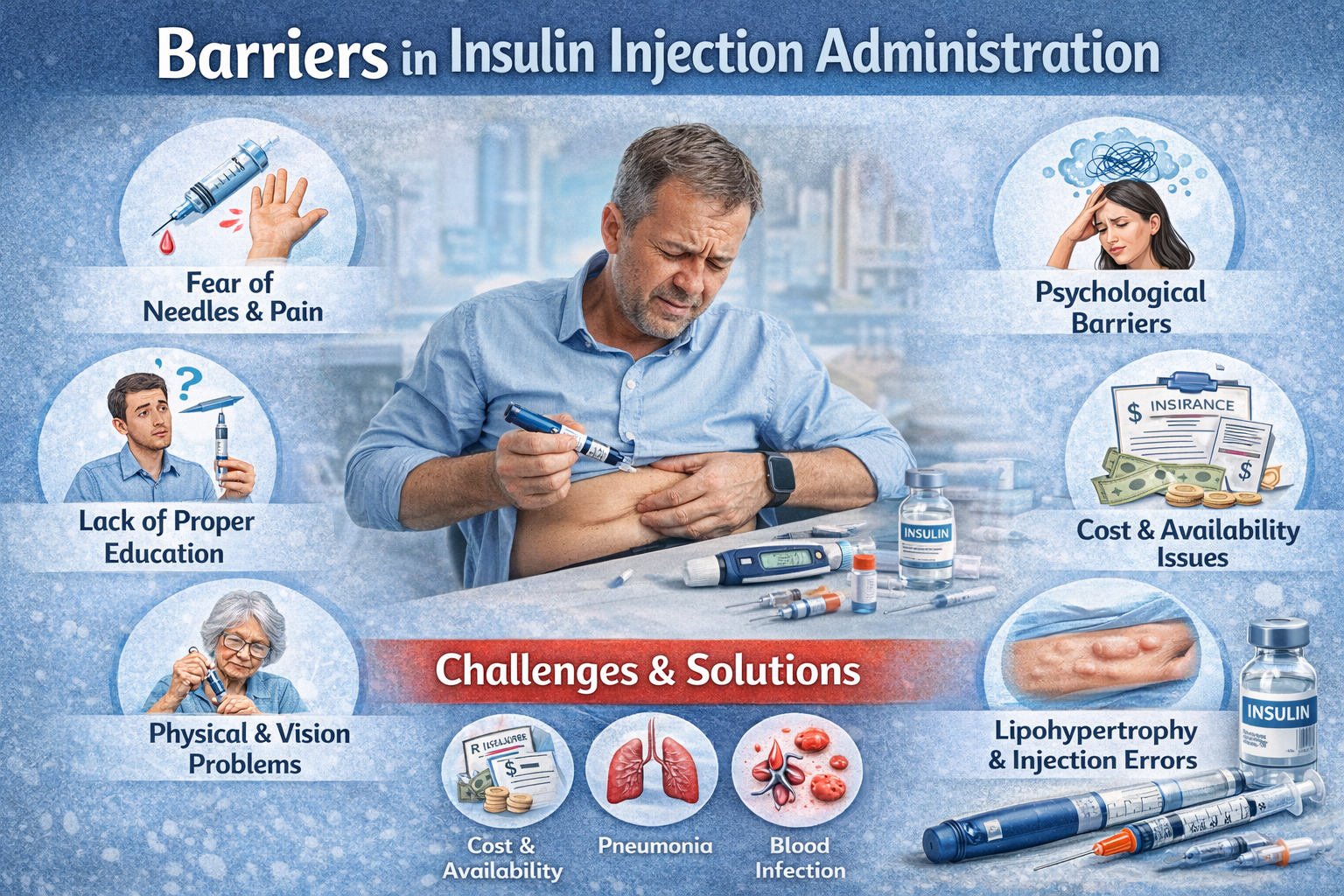
Insulin therapy is a life-saving treatment for people with diabetes, especially those with type 1 diabetes and advanced type 2 diabetes. However, many patients face barriers in insulin injection administration, leading to missed doses, incorrect technique, and poor glycemic control. Identifying and addressing these barriers is crucial for effective diabetes management and prevention of complications.
Common Barriers in Insulin Injection Administration
1. Fear of Needles and Pain
One of the most common barriers is needle phobia. Many patients fear pain, bleeding, or injury from injections, which leads to avoidance or delayed insulin use.
2. Lack of Proper Education
Inadequate training on insulin injection technique can result in:
- Incorrect injection sites
- Improper needle angle
- Failure to rotate injection sites
This reduces insulin absorption and effectiveness.
3. Psychological Barriers
Psychological insulin resistance includes:
- Fear of lifelong dependency
- Feelings of failure or stigma
- Anxiety and depression
These factors often delay insulin initiation and adherence.
4. Poor Injection Technique
Incorrect administration such as injecting into muscle, reusing needles, or not priming insulin pens can cause:
- Unpredictable blood sugar levels
- Pain and bruising
- Lipohypertrophy
5. Lipohypertrophy
Repeated injections at the same site can cause fatty lumps under the skin, leading to erratic insulin absorption and poor diabetes control.
6. Cost and Availability Issues
In developing countries, financial constraints, limited access to insulin, syringes, or insulin pens can become major barriers.
7. Physical Limitations
Elderly patients or those with:
- Poor eyesight
- Arthritis
- Tremors
- Neuropathy
may find insulin self-administration difficult.
8. Social and Cultural Barriers
Some patients feel embarrassed to inject insulin in public or at work. Cultural myths and misinformation about insulin can also prevent proper use.
Consequences of Poor Insulin Administration
Failure to overcome these barriers may result in:
- Poor glycemic control
- Frequent hypoglycemia or hyperglycemia
- Increased risk of infections
- Diabetic ketoacidosis (DKA)
- Long-term complications (neuropathy, nephropathy, retinopathy)
Strategies to Overcome Barriers
Patient Education
- Teach correct injection technique
- Demonstrate site rotation
- Explain insulin storage and needle disposal
Use of Modern Devices
- Insulin pens
- Shorter and thinner needles
- Needle-free injection devices
These reduce pain and improve compliance.
Psychological Support
- Counseling and reassurance
- Address myths and fears
- Family involvement in care
Regular Injection Site Examination
Healthcare providers should routinely check injection sites for lipohypertrophy and guide patients accordingly.
Financial and Social Support
- Use of affordable insulin options
- Government or NGO support programs
- Workplace awareness to reduce stigma
Role of Healthcare Providers
Doctors, nurses, diabetes educators, and laboratory professionals play a vital role in:
- Early identification of barriers
- Continuous education
- Monitoring adherence
- Improving patient confidence
Conclusion
Barriers in insulin injection administration are common but manageable. Through proper education, psychological support, correct technique, and access to affordable resources, patients can overcome these challenges and achieve optimal diabetes control. Addressing these barriers not only improves blood sugar levels but also enhances quality of life.