Winter can be a challenging season for people living with diabetes. Many patients notice higher blood sugar levels and poor diabetes control in winter, even when they follow their usual treatment plan. Cold weather affects physical activity, eating habits, immunity, and insulin sensitivity, all of which can worsen glycemic control. Understanding why this happens and how to prevent it is essential for maintaining good health during the colder months.
Why Does Diabetes Control Worsen in Winter?
1. Reduced Physical Activity
Cold temperatures discourage outdoor exercise. Reduced movement lowers insulin sensitivity, causing blood glucose levels to rise.
2. Increased Caloric Intake
Winter cravings for high-carbohydrate and fatty foods, warm desserts, and sugary drinks contribute to elevated blood sugar levels.
3. Hormonal Changes Due to Cold
Cold weather triggers stress hormones like cortisol and adrenaline, which increase glucose production by the liver, leading to winter hyperglycemia.
4. Higher Risk of Infections
Flu, chest infections, and common colds are more frequent in winter. Infections raise blood sugar levels and can lead to poor diabetes control.
5. Reduced Sunlight and Vitamin D Deficiency
Lower sunlight exposure may reduce vitamin D levels, which is linked to insulin resistance and poor glycemic control.
Health Risks of Poor Diabetes Control in Winter
Uncontrolled diabetes during winter can lead to serious complications, including:
- Frequent hypoglycemia or hyperglycemia
- Increased risk of diabetic ketoacidosis (DKA)
- Worsening of heart disease and hypertension
- Increased frequency of infections
- Delayed wound healing
- Nerve pain and foot complications
Signs of Poor Diabetes Control in Winter
Common warning signs include:
- Persistently high fasting or post-meal blood sugar
- Frequent urination and excessive thirst
- Fatigue and weakness
- Blurred vision
- Increased hunger
- Recurrent infections
How to Control Diabetes Effectively in Winter
1. Maintain Regular Physical Activity
Indoor exercises such as walking indoors, stretching, yoga, or resistance training can help maintain insulin sensitivity.
2. Follow a Balanced Winter Diet
- Choose high-fiber foods
- Avoid excessive sweets and refined carbohydrates
- Include warm, healthy meals like soups with vegetables
- Control portion sizes
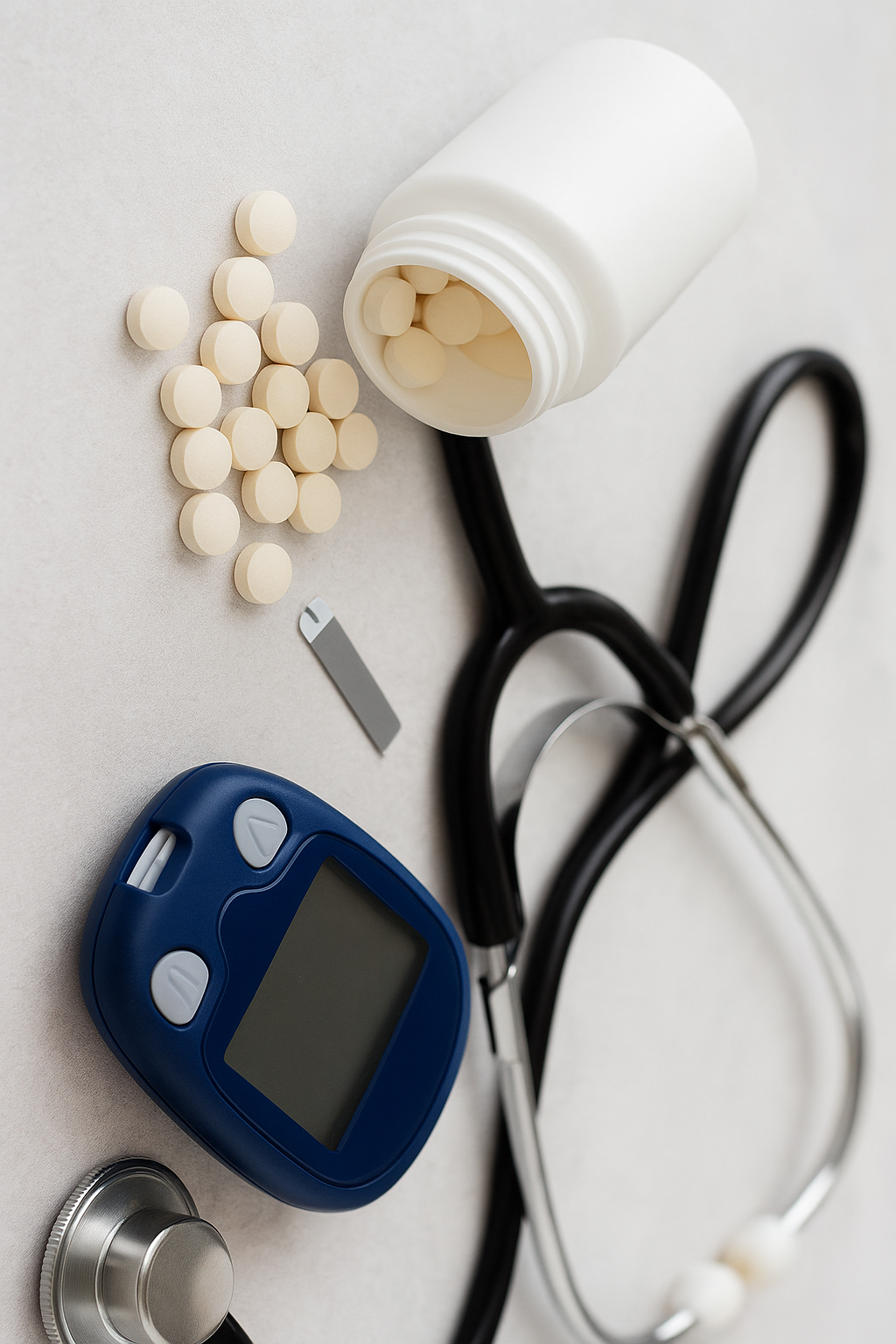
3. Monitor Blood Sugar Frequently
Cold weather and infections can cause unexpected glucose fluctuations. Regular monitoring helps timely dose adjustment.
4. Stay Hydrated
People often drink less water in winter, increasing blood sugar concentration. Adequate hydration is essential.
5. Manage Infections Promptly
Early treatment of flu, cough, or urinary infections can prevent sudden blood sugar spikes.
6. Continue Medications and Insulin Properly
Never skip medications. Insulin should be stored at recommended temperatures, as extreme cold can affect its potency.
7. Get Adequate Sunlight and Vitamin D
Short daily sun exposure or supplementation (as advised by a doctor) may improve insulin sensitivity.
Special Tips for Diabetic Patients in Winter
- Keep feet warm and dry to prevent infections
- Avoid walking barefoot
- Get annual flu vaccination
- Check blood pressure and lipid profile regularly
- Follow sick-day rules for diabetes
When to Consult a Doctor
Seek medical advice if you experience:
- Persistent high blood sugar despite treatment
- Frequent hypoglycemia
- Signs of infection
- Sudden weight loss or extreme fatigue
Early intervention can prevent serious complications.
Conclusion
Poor diabetes control in winter is a common but preventable problem. With proper lifestyle modifications, regular monitoring, balanced nutrition, and adherence to treatment, diabetic patients can maintain stable blood sugar levels throughout the colder months. Winter should be managed wisely to protect long-term health and prevent complications.