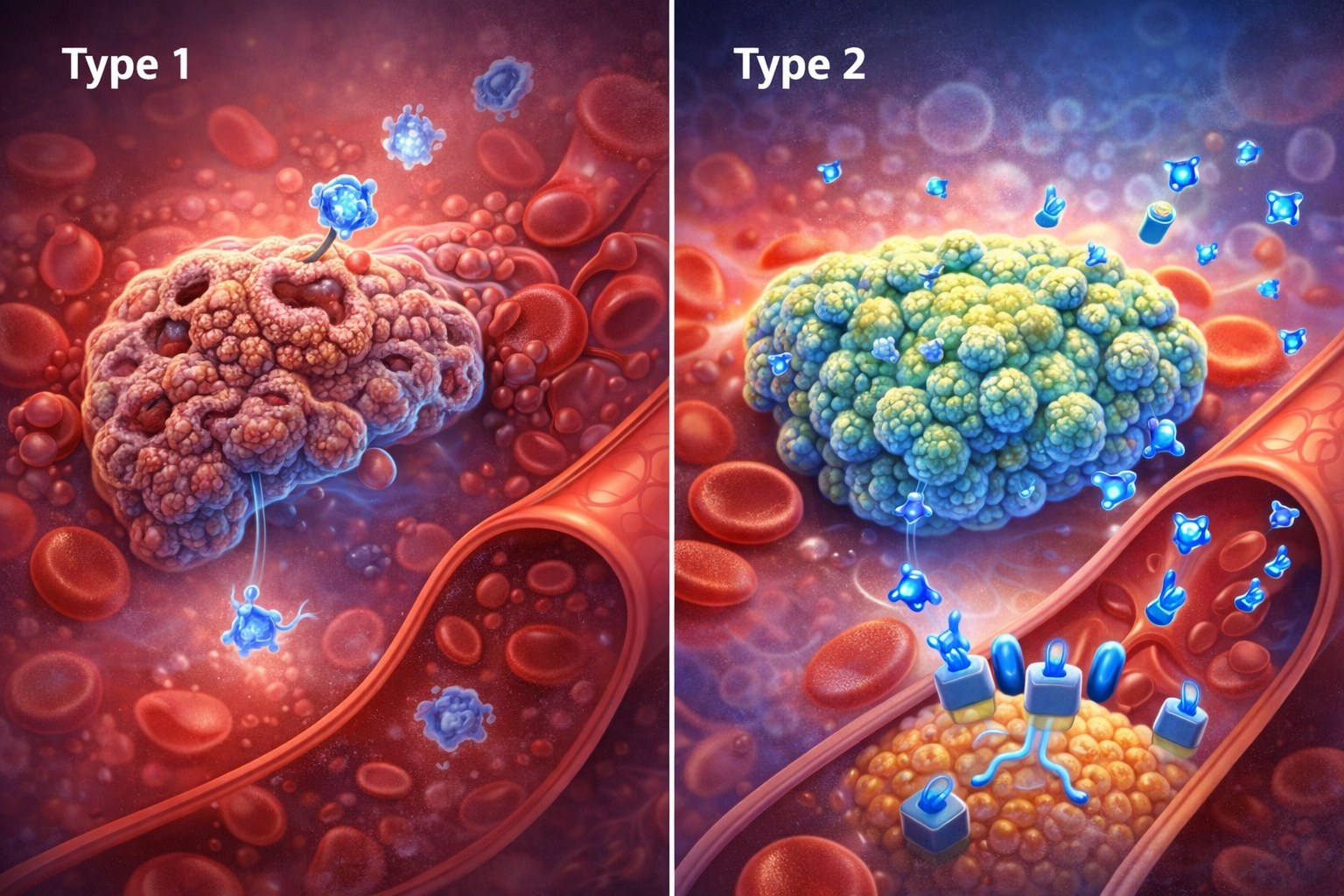
Diabetes mellitus is a chronic condition that affects how the body uses blood sugar (glucose). The two most common forms are Type 1 diabetes and Type 2 diabetes. Although both result in high blood sugar levels, their causes, treatment, and progression are very different. Understanding the difference between Type 1 and Type 2 diabetes helps patients manage their condition more effectively.
What Is Type 1 Diabetes?
Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. As a result, the body produces little or no insulin.
Key Features of Type 1 Diabetes
- Usually develops in children and young adults
- Sudden onset of symptoms
- Insulin is required for life
- Not preventable
- Less common than Type 2 diabetes
What Is Type 2 Diabetes?
Type 2 diabetes occurs when the body becomes resistant to insulin or does not produce enough insulin to maintain normal blood sugar levels. It is strongly linked to lifestyle and genetic factors.
Key Features of Type 2 Diabetes
- Commonly affects adults, but increasingly seen in youth
- Develops gradually
- Often managed initially with diet, exercise, and oral medicines
- Can sometimes be prevented or delayed
- Most common form of diabetes
Main Differences Between Type 1 and Type 2 Diabetes
| Feature | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune destruction of insulin-producing cells | Insulin resistance and reduced insulin production |
| Age of Onset | Childhood or young adulthood | Usually adulthood |
| Insulin Production | Absent or very low | Reduced or ineffective |
| Treatment | Insulin injections required | Lifestyle changes, oral drugs, ± insulin |
| Prevention | Not preventable | Often preventable |
| Body Weight | Often normal or underweight | Often overweight or obese |
| Onset | Sudden | Gradual |
Symptoms of Both Types
Common symptoms include:
- Frequent urination
- Excessive thirst
- Increased hunger
- Fatigue
- Unexplained weight loss
- Blurred vision
Type 1 diabetes symptoms usually appear suddenly, while Type 2 diabetes symptoms develop slowly and may go unnoticed for years.
Treatment Approaches
Treatment of Type 1 Diabetes
- Multiple daily insulin injections or insulin pump
- Regular blood glucose monitoring
- Balanced diet and physical activity
- Education on hypoglycemia prevention
Treatment of Type 2 Diabetes
- Healthy diet and weight control
- Regular physical activity
- Oral antidiabetic medications
- Injectable medications or insulin (if needed)
Complications in Both Types
If not properly managed, both types can lead to:
- Heart disease and stroke
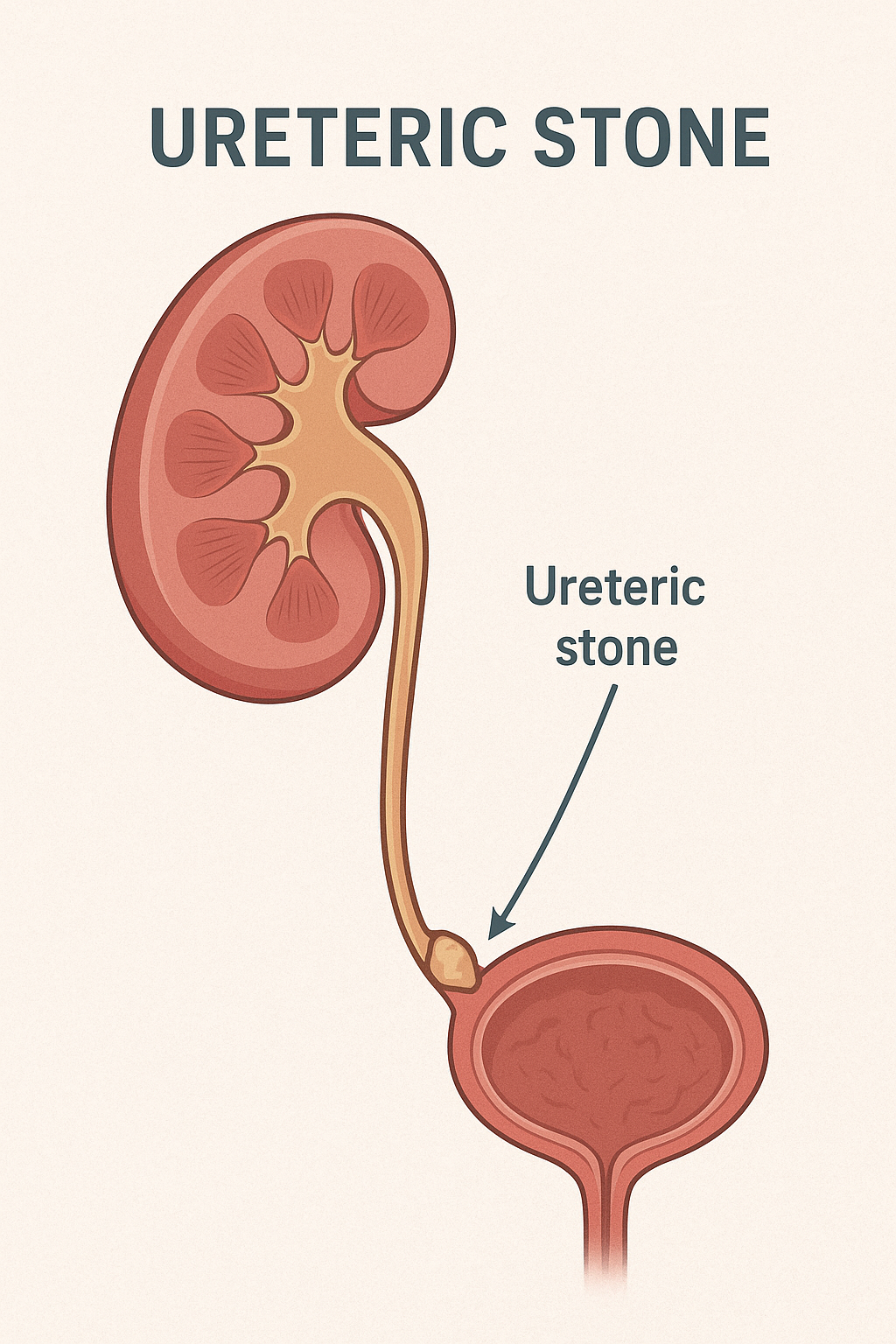
- Kidney damage
- Eye problems (diabetic retinopathy)
- Nerve damage
- Foot complications
Good blood sugar control significantly reduces these risks.
Can Type 1 Turn Into Type 2 Diabetes?
No. Type 1 and Type 2 diabetes are distinct conditions. However, a person with Type 1 diabetes can develop insulin resistance, a condition sometimes referred to as “double diabetes.”
Conclusion
While Type 1 and Type 2 diabetes share common symptoms and complications, their causes and management strategies differ greatly. Type 1 diabetes requires lifelong insulin therapy, whereas Type 2 diabetes can often be managed and sometimes prevented through lifestyle changes and medications. Early diagnosis, education, and regular medical follow-up are essential for living a healthy life with diabetes.